Prince George Healthcare Center in Georgetown has been cited because “the facility failed to make sure that the nursing home area is free from accidental hazards and risks and provides supervision to prevent avoidable accidents.” Because of this, a resident was put in immediate jeopardy.
According to the inspection report, the resident often wanders around the facility. She also often tries to leave the facility, “attempts to void in inappropriate places/trash cans,” and “prefers to sleep on [the] couch in the main area at times.”
With the resident’s needs in mind, the goal of her care plan was to “let her wander safely within specified boundaries.” The approaches listed in the resident’s care plan to attain this goal were to:
- Remove the resident from others’ rooms and unsafe situations when she wandered.
- Approach the resident from the front and walk in step with her before redirecting her.
- Provide the resident with activities based on her prior lifestyle, like folding towels.
- When resident begins to wander, provide comfort measures to make sure her basic needs (i.e. pain, hunger, toileting, etc) are being taking care of.
On multiple occasions, the resident was combative and redirection was unsuccessful. She often wandered in and out of other residents’ rooms, tried to undress, looked for exits, and ran down halls, sometimes with her pants around her ankles. Staff had difficulty redirecting her, and ended up having to medicate her to go back to bed on many occasions.
On on occasion, the resident attempted to find exits several times. The alarms sounded and staff were able to stop her, but it was very difficult to redirect her. Another time, she was wandering the halls in just briefs and shirt looking for exits. She held the door until the alarm sounded, then would try another exit down the hall until that alarm would sound. Sometimes she was easily redirected, and others she was very difficult.
According to the incident report, she wandered into a day room and removed her pants over a trashcan. She was redirected to her own room by staff. This same shift she was redirected from several other rooms, but was not combative. It wasn’t uncommon for her to try to take her clothes off, which was sometimes resolved after toileting. She was often confused and in others’ rooms, but not combative and didn’t affect anyone directly.
However, this wasn’t always true. The resident was, in multiple instances, combative and put herself and other residents at risk.
According to the report, the resident had chased a staff member out of a room agitated, forcefully grabbed the arm of a visitor, and been combative during care from nursing home staff. She had wandered from room to room, tried to push a resident out of their own room and scratched their hands before being redirected, upsetting the other resident.
Another incident reported the resident running down the hall and into a room where she hit her head on a door, resulting in a laceration above her left eye. Staff applied sterile strips and reported no other injuries. Later that day, the resident was running around the unit again, very unsteadily. She was looking for exits, entering others’ rooms, rummaging through drawers and was very difficult to redirect.
Another day, the resident tripped over a wheelchair when running in a day room. Nurses reported she did not hit her head and had no apparent injuries. They attempted to get her to wear a safety helmet, to which she refused, though she wore elbow and knee pads when tolerated.
In another incident, after making several exit attempts, the resident was running up and down the halls and in and out of other residents’ rooms. She later defecated on the floor.
A few days later, a nurse heard screaming from the resident’s room. Her roommate was on the floor, resident standing nearby. The resident’s roommate said “I was going to come out of the room and come down to the dining room when she came behind me and pushed me down.” When asked if she had pushed her roommate down, the resident mumbled indistinctly and did not answer the question directly. The nurses separated the residents.
Later that day, the resident refused incontinence care twice. Visibly agitated and anxious, she went to sit in a dining chair, tipping over. Nurses report she did not hit her head or sustain any other injuries.
The resident had shown the need for close supervision multiple times, causing distress and harm to herself and others. These accidents could have been easily prevented if the nursing home facility had placed this resident under closer supervision.
Prince George Healthcare Center has also been cited for failure to “provide and implement an infection prevention and control program.” The facility’s violations involved improper catheter care hygiene, improper contact precautions, wound care contamination and placing respiratory care materials on the floor. This is especially pertinent today in the age of COVID-19. The facility has had at least one confirmed case of COVID-19.
Don’t Wait. Get Help for Nursing Home Abuse Today.
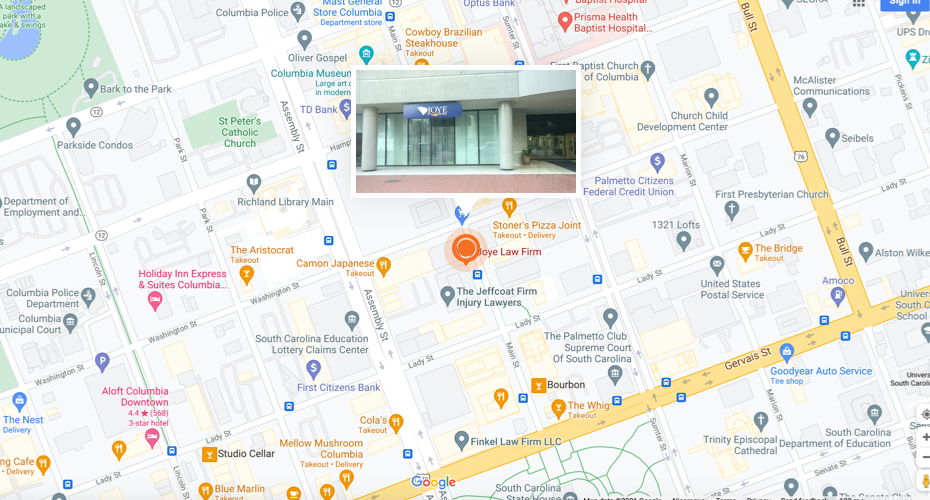
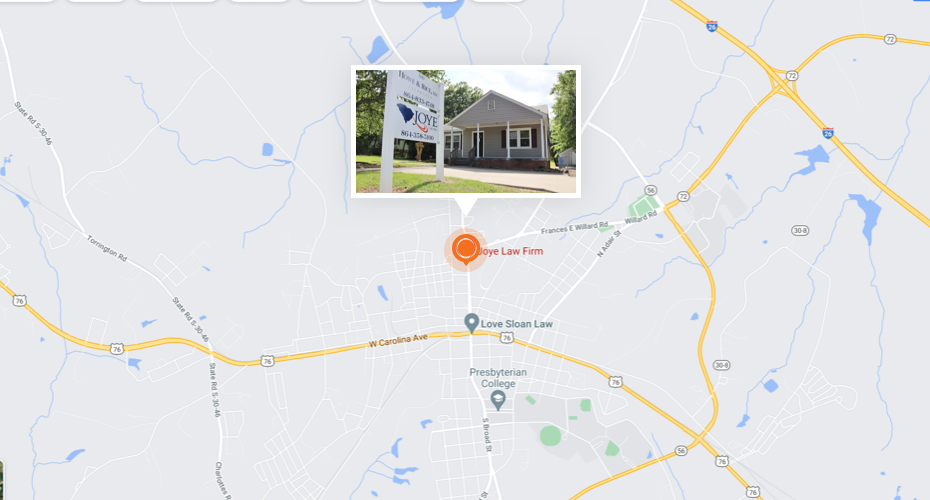
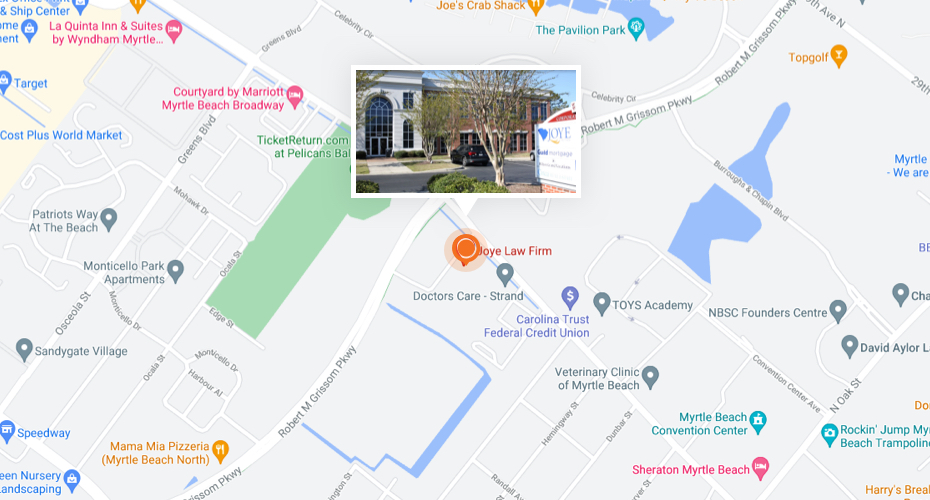
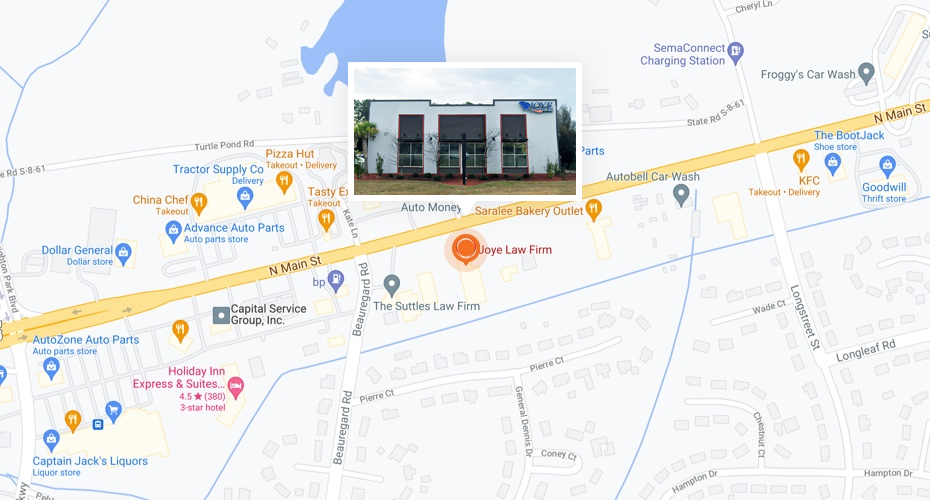
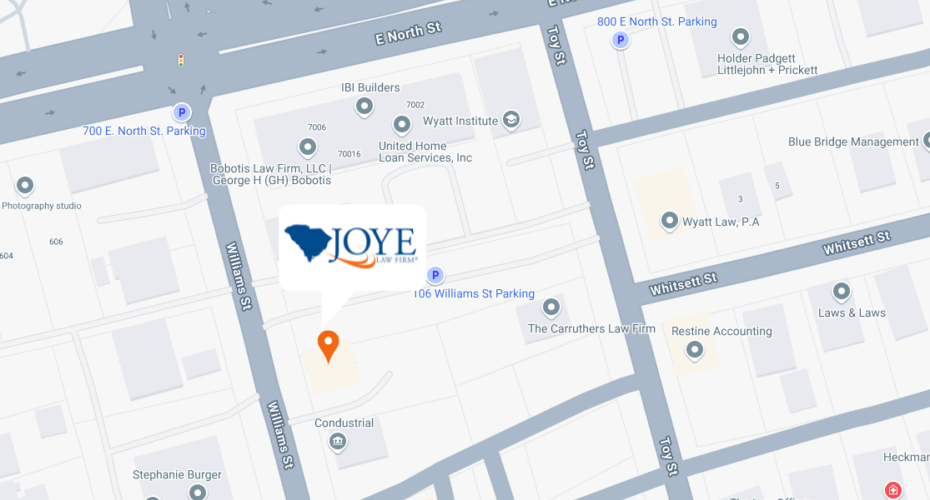
If you suspect nursing home abuse, we will provide a free, confidential case evaluation with no obligation to hire us. With nearly 250 years of shared experience, Joye Law Firm attorneys are consistently recognized by clients and peers at the highest level of professional excellence. We make sure to fight hard for our clients and are honest with them every step of the way.